My own experience of being sent to a hospital began with what, in hindsight, was a relatively simple breakdown. Being a 17-year-old living alone in a foreign country, I was overwhelmed, struggling to keep up, and needed emotional support. At my school, the policy was clear: any concern, big or small, can be discussed with the counselor. At the very beginning of the school year, students are encouraged to treat counselors as the catch-all solution.
It was a September afternoon, a fine day with a crisp chill in the air and still touched by the warmth of sunlight. Yet, my spirits had plummeted to a low ebb. Emotionally overwhelmed, I decided to reach out to the school counselor for help. Upon arrival at her office, I started talking about how I was not getting along with my roommate and how I was struggling with a lot of AP courses, among other challenging yet common high school kid’s concerns. Without even trying to comfort me in any way, I was handed an evaluation form to fill out. With no instructions about why it mattered, what options existed, or what would happen next from my counselor, I filled out the form to my best guess. After submitting it, I heard nothing until I was told I would be sent to a hospital for “treatment.”
On the way to the hospital, I was told that the “treatment” and evaluation would be more thorough and targeted. Trusting school and my counselor, I left my guard down and believed that going to the hospital was necessary. However, I asked the houseparent if I could talk to my parents and explain that I was being sent to the facility. “No, we will call your parents and explain the situation to them.” I was told. Until then, things seemed to go as planned, and I was on the way to getting professional help that would help me feel better.
Upon arrival at the hospital, I waited for hours before being seen, sitting in a crowded intake area with other patients. Seeing that the staff at the hospital were actually very friendly, I even had a little relief and a sense of belonging, and I felt that I had found a place that could support me. However, the first thing that happened was that staff took away my phone, my clothes, and even personal items, without any explanation. For someone already anxious, the sudden loss of control and contact with family and my personal belongings is terrifying. It was at that moment that I realized that I was being sent to a mental health institution.
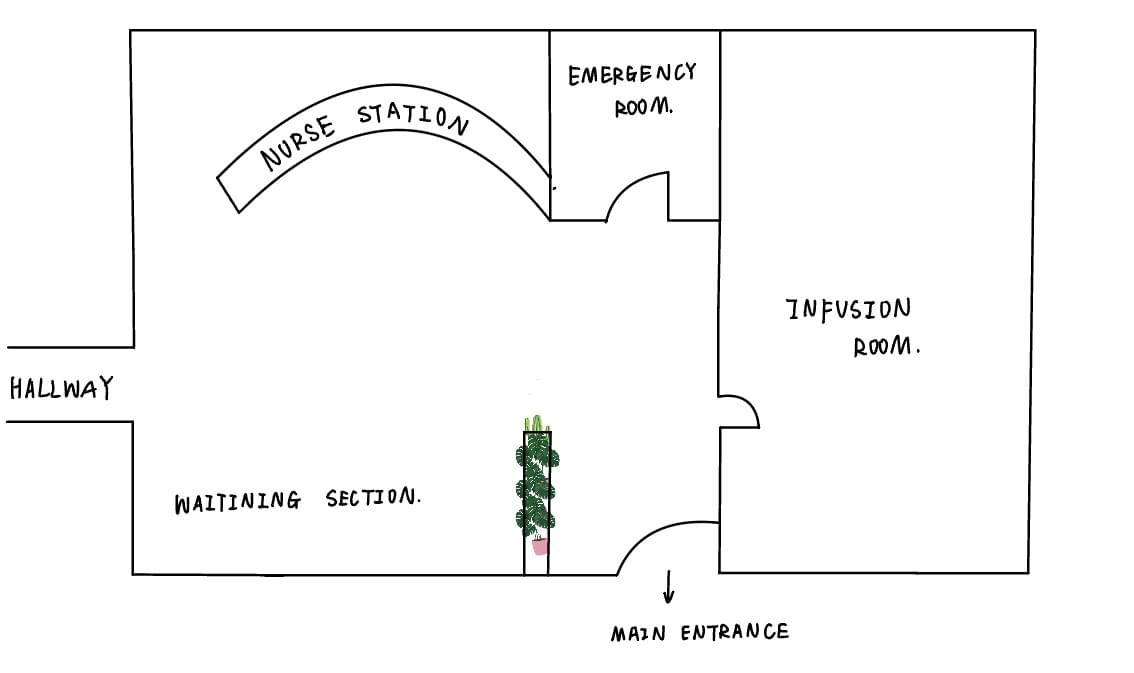
Graph 1: layout of the main entrance of the emergency section
I rarely cry out of fear. However, when the guards took away all my mobile phones, headphones, power banks, food, coats, backpacks, etc., and when I walked in and saw a large number of mentally ill patients, I broke down. Surrounded by other patients, I was so frightened, terrified, unsure that I started to question myself and my trust in the people around me. I even begged a nurse to put me in a separate room and to give me my phone so I could communicate with my parents. I thought about how long I would have to be afraid of and when this long night would end.
After almost 6 hours of waiting, I finally saw a doctor. The meeting was short, and the encounter felt routine and impersonal. The doctor did not prescribe any drugs or even allow me to take my own prescription. “You sounded fine. “You can go,” were the few words he said to me. It is safe to say that I did not receive the “better evaluation” that the school promised. It appears that having treated dozens of similar cases, the doctor relied on a standardized script and did not see the need to offer substantial evaluation or physical check-up. I felt processed, not cared for. What had started as a moment of personal vulnerability had now escalated into hospital admission that left me feeling mistrusted and invisible.
Analysis of Process-based Healthcare System
My experience of being sent to a hospital without my permission or understanding shows that there are bigger problems with how institutions deal with mental health crises, especially for students and minors.
First, the evaluation process was unclear and the same for everyone, putting liability ahead of care. I didn't get clear explanations about the form I was filling out. Instead, I was moved through a system that saw me as a liability to manage rather than a person in need of help. Studies show that not being open and involved like this hurts patients' ability to make their own decisions. A 2020 review on consent in psychiatry emphasizes that genuine informed consent necessitates disclosure, capacity evaluation, and voluntarism, standards frequently overlooked in psychiatric settings (PMC, 2020). In the same way, WHO's QualityRights guidance (2021–2023) says that mental health services should be based on dignity, autonomy, and rights. This goes against the kinds of coercive processes I went through.
Second, the role of liability was more important than the role of care. My school decided to send me to the hospital right away, which seemed more like a way to protect itself from risk than a way to help me. My parents were pulled into the process only after the fact. Instead of a supportive conversation, their meeting with school administrators felt like bargaining over liability. The school positioned hospitalization as necessary to protect me from harming myself and itself, while my parents questioned whether it was an overreaction. What could have been an open, supportive evaluation became an adversarial process. This is in line with criticisms in the AMA Journal of Ethics (2024), which say that institutions often put metrics of risk management and bed counts ahead of patient-centered standards like trust, healing, and autonomy.
Thirdly, there weren't enough staff or resources at the school or the hospital. My six-hour wait in the intake area and the lack of any assessments were part of a bigger problem with psychiatric "boarding" in emergency departments. Reviews in the Mayo Clinic Proceedings and the American Academy of Pediatrics (AAP) show that these long waits make symptoms worse, make safety risks higher, and make stays longer for both adults and children. For minors, the harms are magnified: low night-shift staffing is associated with sleep disruption, fear, and reduced feelings of safety (Sandelin et al. 2020). A 2020 PubMed study on night ward experiences found that when staffing is low and supervision is impersonal, young people are more likely to be scared, have trouble sleeping, and feel more vulnerable.
It is clear what the main problem is in all of these areas: getting healthcare does not always mean getting good care. Institutions frequently regard patients as mere data points within a process or as issues requiring resolution, rather than recognizing them as individuals deserving of empathy, transparency, and autonomy. My experience aligns with the concept of "catastrophic care gaps" as defined by WHO (2023), wherein formal systems are in place, yet patients face obstacles related to process, cost, or neglect that render services ineffective in practice.
Process-focused Healthcare System vs. Patient-based Healthcare System
These systemic deficiencies have profound consequences. Patients lose trust in institutions. When my counselor grew impatient without explanation, and when hospital staff confiscated my belongings without clarity, I felt unsafe and mistrustful. This mirrors findings from systematic reviews of seclusion and restraint: patients consistently report feeling punished and stripped of dignity (Chieze et al. 2019).
This lack of trust doesn't go away easily. Research on minors indicates that consent and autonomy are particularly vital:58% of high school students in one study refrained from seeking mental health care due to concerns regarding parental consent, and 25% stated they would not pursue assistance if confidentiality could not be assured (JCHC, 1993). For students like me, the lack of clarity and autonomy in school-to-hospital pipelines may discourage future help-seeking, exacerbating crises over time. There are also safety risks that come with losing a patient's trust. When patients stop going to institutions, they might put off getting care until their condition gets worse or not tell their doctors about important symptoms. The World Health Organization (WHO) says that coercive practices in psychiatry raise the risk of trauma and suicidal thoughts instead of lowering them. This means that systems that are supposed to make people "safe" may actually make things worse, hurting both people's health and public health goals. Recent scholarship echoes this:Taylor & Francis (2024) reports that adolescents are more likely to engage with treatment when informed consent frameworks respect their autonomy.
Finally, the patient and the system stop working together and start working against each other. I felt like administrators, parents, and clinicians were all trying to get what they wanted from me instead of supporting me. My voice was the least important in the room. These kinds of interactions go against the idea of person-centered care, which is based on recovery, working together, and rights (PMC, 2020). Without these things, mental health facilities could become places of fear instead of healing.
Policy Proposals
One simple thing that could really help people like me is to make school-to-hospital mental health referrals more open and focused on young people. The main issue in my case was not just that I was sent to the hospital, but that I didn't understand why, didn't have a say in the process, and didn't have a chance to have a say in decisions about my care. Schools and hospitals should use consent frameworks that are in line with the Mature Minor Doctrine and WHO's Quality Rights initiative. This will make sure that teens are treated as partners instead of passive subjects. This would mean that counselors would have to use plain language to explain evaluation tools, list the possible next steps (including hospitalization), and get the student's agreement as well as the parent's. Studies on adolescent confidentiality indicate that when youths perceive themselves as informed and valued, they are more inclined to participate in treatment and less inclined to evade care (JCHC, 1993; Taylor & Francis, 2024).
These kinds of protocols are cheap and can be put into place right away. To have a patient-based healthcare system and not simply a system focusing on process doesn't require investments in new buildings or medical equipment; all they need is training for staff and the use of standard communication methods. Transparent consent would change a process that now feels forced into one that builds trust, restores dignity, and gives students power. Schools and hospitals could stop the isolation and mistrust that often follow mental health referrals by focusing on communication and agency. This would make care not only available but also meaningful.
Bibliograph
American Academy of Pediatrics. 2022. “State-by-State Variability in Adolescent Privacy Laws.” Pediatrics. Elk Grove Village, IL: AAP Publications.
American Medical Association. 2024. “Why Patient-Centered Built-Environment Standards Matter.” AMA Journal of Ethics.
Anyangwe, Stella C. E., and Chipayeni Mtonga. 2007. “Inequities in the Global Health Workforce: The Greatest Impediment to Health in Sub-Saharan Africa.” International Journal of Environmental Research and Public Health 4 (2): 93–100.
BioMed Central. 2023. “Existential Impact of Seclusion: A Thematic Analysis.” BMC Psychiatry.
Frontiers in Psychiatry. 2021. “Systematic Review of Built Environment and Outcomes in Inpatient Mental Health Facilities.” Frontiers in Psychiatry.
Frontiers in Psychiatry. 2022. “Law and Psychiatry—Current and Future Perspectives.” Frontiers in Psychiatry.
HFM Magazine. 2017. “Designing with Dignity in Pediatric Behavioral Health Facilities.” Health Facilities Management.
HKS Architects. 2023. “How Design Supports Improved Pediatric Mental and Behavioral Health Outcomes.” HKS, Dallas, TX.
Mayo Clinic Proceedings. 2019. “Psychiatric Boarding and Patient Outcomes: National Clinical Review.” Mayo Clinic Proceedings.
National Institutes of Health. 2015. “Informed Consent to Treatment in Psychiatry.” PubMed Central (PMC).
National Institutes of Health. 2019a. “Systematic Review: Effects of Seclusion and Restraint in Psychiatric Settings.” PubMed Central (PMC).
National Institutes of Health. 2019b. “Qualitative Review of Seclusion Experiences.” PubMed Central (PMC).
National Institutes of Health. 2020. “Person-Centred Care and Psychiatry: Key Perspectives.” PubMed Central (PMC).
National Institutes of Health. 2020. “Lived Experience on Psychiatric Wards at Night: Patient Interviews.” PubMed.
New York City Department of Health. 2021. “Mental Health by Design: Student-Designed Wellness Spaces.” Architectural Digest.
Pediatrics. 1993. “Parental Consent as a Barrier to Adolescent Mental Health Services.” Journal of Child Health Care.
Perry, Henry B., Rose Zulliger, and Michael M. Rogers. 2014. “Community Health Workers in Low-, Middle-, and High-Income Countries: An Overview of Their History, Recent Evolution, and Current Effectiveness.” Annual Review of Public Health 35: 399–421.
ScienceDirect. 2024. “Umbrella Review of Psychiatric Hospital Architecture and Design.” ScienceDirect.
Taylor & Francis. 2024. “Independent Adolescent Consent to Mental Health Care: A Policy Review.” Taylor & Francis Online.
UEA Digital Repository. 2019. “Qualitative Review of Seclusion Experiences: Patient Perspectives.” Norwich: University of East Anglia.
United Nations Human Rights Office. 2006. Convention on the Rights of Persons with Disabilities (CRPD). New York: United Nations.
Wikipedia. 2023a. “Mature Minor Doctrine.” Wikipedia.
Wikipedia. 2023b. “TeenScreen: School-Based Mental Health Screening (1999–2012).” Wikipedia.
Wikipedia. 2023c. “Hope Squad: Peer-to-Peer Suicide Prevention.” Wikipedia.
Wikipedia. 2023d. “Trauma-Informed Approaches in Schools.” Wikipedia.
World Health Organization. 2021–2023. WHO QualityRights Guidance and Training Tools. Geneva: WHO.
